The Local newsletter is your free, daily guide to life in Colorado. For locals, by locals.
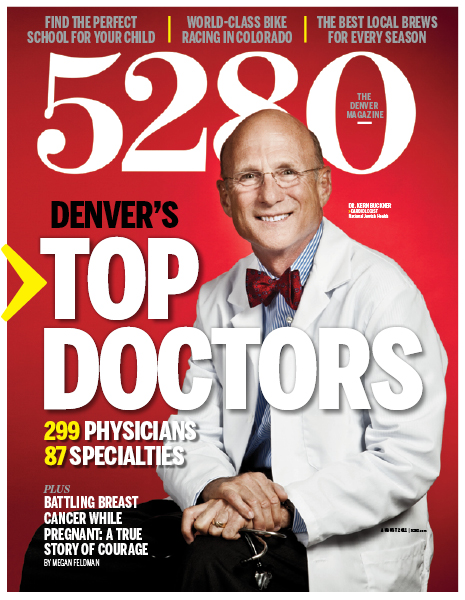
View the list of nearly 300 doctors in more than 80 specialties.
For 18 years, we’ve been distributing ballots, tallying votes, and ultimately, giving you access to the most comprehensive list of the city’s leading doctors. During that time, much has changed in the world of medicine: Surgeries have gone robotic. Infertility has become easier to overcome. AIDS has gone from a death-sentence diagnosis to a chronic disease. Yet some things never change. Medicine, for all its improvements and advances, is still an inexact science, and the pathways to a healthy mind and body often remain elusive for patients and doctors alike. // With that in mind, we asked 10 of this year’s Top Docs to help us understand why health care doesn’t always offer easy answers—even though most Americans expect that nearly everything can be cured with a pill or diagnosed with a simple CT scan. On the following pages, we tell their stories of difficult diagnoses, mysterious diseases, medical miracles, challenging treatment options, and a slew of advice about how patients—and physicians—need to remember that doctoring is often as much art as it is science.
In his new book, Being A Doctor: The Art of Medicine (Outskirts Press 2011), ophthalmologist Dr. Joel Goldstein (a Top Doctor 15 times over) speaks first and foremost to up-and-coming physicians, but his words will resonate with anyone who’s ever waited anxiously in an exam room. “If you don’t know the answer, that’s okay,” he writes. “Patients appreciate honesty. Be comfortable requesting an opinion from another physician, or referring the patient out. No one knows everything, especially in medicine.” Which is a stripped-down way of saying the best course of action isn’t always clear. Sometimes “treatment” means multiple office visits, long discussions, exclusionary tests, trial-and-error diagnoses, additional consults, and a hefty dose of patience while the doctor figures out what might be the correct way to move forward.
These doctors’ anecdotes and advice illustrate very clearly that no matter how sophisticated our medical techniques become, patients and doctors are still just humans. And that’s a good thing because it’s the relationship between those two people that offers an opportunity to be better, seek the correct answers, reason through problems, and work until the patient finds his or her version of good health.
Medical Miracle: Thrown A Curve
When a routine appointment turns into something altogether uncommon—and very scary.
“We’re people of faith,” Christopher Cole says. “So the first thing we did after hearing the results was to pray.” The impulse to solicit help from a higher power was understandable: A large mass had just been found in Cole’s daughter’s chest.
Anna Cole, 10, had gone to see the pediatrician about an increasingly noticeable curvature of her spine. Her parents thought it might be scoliosis. Instead, over the phone, the pediatrician told them the X-rays showed a growth the size of a cantaloupe living in Anna’s lung. It was pulling on her spine. “That’s not the kind of call any parent wants,” says Christopher, a cardiologist practicing in Colorado Springs. “But as a physician, I knew just enough to be very afraid.”
Christopher also knew finding highly qualified physicians for his daughter was the next crucial step. After a CT scan and a needle biopsy yielded little information about the type of mass they were dealing with, the Coles met with an oncologist and a surgeon in the Springs. There were a variety of possible diagnoses: It could’ve been a relatively rare congenital bronchogenic cyst, a malignant growth called a neuroblastoma, or a benign tumor called a ganglioneuroma. No matter what it was, it definitely had to be removed—which is how the Coles ended up in Dr. Steven Rothenberg’s offices at the Rocky Mountain Hospital for Children at Presbyterian/St. Luke’s Medical Center in Denver.
“The doctors in Colorado Springs were good people and good doctors I’m sure,” Christopher says, “but they weren’t offering the care we wanted for our daughter.” More specifically, they weren’t offering to do her surgery any other way besides an open thoracotomy, an invasive surgery that would leave the budding concert pianist with a 14-inch incision, an extended recovery time that would prevent her from playing a much-anticipated recital, and the possibility of developmental deformities as she continued to grow. Like everything else in life—and in medicine—the best course of action wasn’t exactly clear. So, they made a few more phone calls, and found Dr. Rothenberg.
“I’m probably one of the few surgeons in the country who would try to do this exact surgery thoracoscopically,” Dr. Rothenberg says with a sheepish shrug. “I just really thought I could do it.” Instead of opening Anna up from sternum around to her spine, Rothenberg would use four small openings and small surgical tools to do the procedure in a minimally invasive way. To the relief of Anna’s parents, he was correct. He could do it. But it took Rothenberg more than two-and-a-half hours to painstakingly extricate the tumor from her lung and spine. Then the surgeon had to dice the large tumor into small enough pieces to remove it through the four small incisions in Anna’s chest. “At that point we still didn’t know if it was cancerous or not,” Rothenberg says. “I had to use a plastic bag and make sure none of the tumor tissue touched the open incisions. Cancer cells can easily spread that way.”
It took 36 hours for the pathologist’s report to come back. When it did, the Coles learned that the tumor, which had collapsed more than one-third of their daughter’s lung, was not cancerous. It was an unusually large ganglioneuroma that had likely been growing for years, increasing in size slowly enough that Anna’s little body was able to compensate and avoid symptoms. By the time they received the call, Anna was already up and goofing around like a typical 10-year-old. In fact, just one week after Rothenberg made his first incision, Anna sat down in front of 50 people and tickled the ivories. The audience marveled at her—but not everyone knew just how miraculous her performance really was.
Mystery Disease: Breathless
Trying to make sense of a sickness that robs kids of oxygen.
Dr. Robin Deterding is doing her best to get off the phone, but it’s not always easy when you’re responsible for other people’s capacity to breathe. She looks over and mouths a quick I’m sorry before speaking back into the receiver: Well, I mean, he’s growing normally, right? Good. That’s good. But, yes, I’ll take a look. I gotta go right now, though, OK? She hangs up the phone, apologizes again, and says, “So what can I tell you about kids who can’t breathe?”
Deterding is a pediatric pulmonologist and the director of the Children’s Breathing Institute and Interstitial Lung Disease Program at Children’s Hospital Colorado. She sees patients with a range of breathing-related issues—everything from asthma and cystic fibrosis to airway anomalies and pneumonia. But her phone rings often these days with questions about a disease she’s spent the last 16 years trying to decode: neuroendocrine cell hyperplasia of infancy (NEHI).
“Now I get calls from all over the world,” the doctor says, explaining that she’d recently spoken on the phone with someone in Finland. “But back in 1995, when we first began noticing patients with these symptoms, no one believed us.” No one believed, that is, that Deterding and her mentor, Dr. Leland Fan, were seeing a disorder that caused very sick babies and toddlers to breathe fast and require oxygen therapy—because when a lung biopsy was performed, nothing appeared to be wrong.
That didn’t sit well with Deterding; she knew something was causing these kids to be sick. Something other than asthma, a virus, or pneumonia—illnesses for which most of these children had been previously diagnosed and unsuccessfully treated. So Deterding and her colleagues began gathering lung tissue samples and sent them to a pathologist in Texas. The findings were surprising—and confusing. “These kids had too many neuroendocrine cells in their lungs,” Deterding says, explaining that those types of cells usually aren’t present after six months of age. “But to this day, we don’t know why they have these cells, or how the cells are involved in making the children sick.”
And the kids are very sick. They breathe 50 percent faster than most children their age. They experience poor weight gain. And they almost always require extra oxygen, sometimes until they are as old as six. The current treatments for the symptoms of the disease are limited to oxygen and a high-calorie diet. But Deterding and her colleagues are hoping to offer better solutions in the near future. “We’re collecting clinical material and working with the top scientists in the world,” Deterding says. “I think we have some good clues to figure this out.”
Difficult Diagnosis: Sugar High
How one incorrect medical conclusion can come crashing down years later.
It was only four days until the wedding, and Renee Miller and Christopher Bevis* were running from one prenuptial engagement to the next in their hometown of Mt. Adams, Ohio. The parties and showers were all in good fun, but the bride- and groom-to-be were both exhausted. Which is why Renee wasn’t overly concerned when her fiancé got dizzy climbing the stairs to his condo and almost fell backward. “At the time, I really didn’t think there was anything seriously wrong with him,” she says. “Christopher had been trying to lose weight for the wedding, and he had not been eating enough since we were so busy.”
Christopher wasn’t as sure, so he scheduled a physical exam for later that day. After all, they were leaving for a two-week honeymoon; he didn’t want to feel bad the entire time. Renee met Christopher back at his condo after the appointment. “When he sat me down on the couch,” Renee says, “I knew I had been wrong about all this being a consequence of his efforts to lose weight.”
Her six-foot-six-inch, 240-pound fiancé had come home with a diagnosis of Type II diabetes. His blood sugar was well over 600 milligrams per deciliter (anything over 200 mg/dL is considered diagnostic for diabetes). And he was experiencing diabetic ketoacidosis, a medical emergency that can lead to decreased blood pressure, cerebral edema, circulatory failure, and acute respiratory distress. In other words, Christopher was pretty darn sick. But the doctor had explained the disease, prescribed medication, and sent Christopher home to his bride-to-be.
For the first two years of their marriage, Christopher lived in what Renee describes as a living coma. He was agitated, foggy, and fatigued. His vision sometimes blurred. He slept all the time, going to bed most nights before 6 p.m. He experienced memory loss. No matter what medication at whatever dosage he tried, Christopher never felt any better. Even with a strict diet of chicken, fish, and vegetables, and an exercise plan that included walking after dinner every night, the Bevises’ diabetic nightmare continued. Everyone had told Renee the first years of marriage were the hardest; she was quite certain it wasn’t supposed to be this difficult.
When the couple learned of an opportunity to move to Denver with Renee’s job in late 1998, they took it. Christopher had spent his childhood in Littleton, and Renee had family in Denver. It seemed like a good opportunity to refresh their lives. After six months in Colorado, Renee took a job with a different organization, Takeda Pharmaceuticals North America Inc., partly because the company focuses on a variety of therapeutic areas, including diabetes. “I wanted to learn about diabetes desperately,” she says. “I wanted to dissect the disease. This job was going to help me help Christopher.”
But months passed, and although Renee was learning much about the disease, she hadn’t learned anything that would help her ailing husband. That is, until she started meeting with doctors, specifically endocrinologist Dr. Satish Garg at the Barbara Davis Center for Childhood Diabetes.
One day after mentioning her husband’s uncontrolled illness to Dr. Garg, the Bevises found themselves waiting on test results in one of the center’s patient rooms. “We had been waiting for a while when Dr. Garg and a nurse came into the room with a needle and syringe,” Renee says, recalling that her first thought was that they’d already taken many vials of Christopher’s blood. Christopher told the nurse he didn’t think he had any blood left to give her. The nurse smiled and said she didn’t need to take any more blood. The syringe was full of insulin.
Christopher didn’t have Type II diabetes. He had Type I diabetes. And he needed insulin immediately.
“Type I and Type II diabetes are completely different diseases,” says Dr. Michael McDermott, who has been Christopher Bevis’ doctor since shortly after the correct diagnosis was made at the Barbara Davis Center. “About 95 percent of Americans who have diabetes have Type II. But that leaves five percent that need to be treated very differently.” McDermott, who is the director of the endocrinology and diabetes practice at University of Colorado Hospital and is well-known for diagnosing former Broncos quarterback Jay Cutler’s Type I diabetes, says incorrect diabetes diagnoses are on the rise.
For decades, anyone who came in with symptoms as a child was diagnosed with Type I diabetes, which is the insulin-dependent variation of the disease. Anyone who visited the doctor with symptoms as an overweight adult over 40 was tagged with Type II. “But these days, with children becoming more and more obese, we have to recognize that you can’t just look at a person and make a diagnosis,” the doctor says. “These diseases are the single highest cause of kidney failure, blindness, and limb amputation, and the strongest risk factor for heart attack among Americans. We can’t miss diagnosing it correctly, especially when all it takes is a blood test.”
And that’s all it took for the Bevises. That, and a vial of insulin. “To this day, Christopher remembers the feeling as if it was a minute ago,” Renee says. “He said the fogginess and blurriness disappeared almost immediately. As the morning progressed, he felt more awake, more energetic, and more alive. Christopher was waking up again and hadn’t been that alert in years. My husband was back.”
Difficult Diagnosis: Brain Teaser
How a simple headache becomes complicated in the blink of an eye.
You don’t have to work in health care to know that much of what rolls through emergency room doors isn’t emergencies. That can be especially true when the patients are children: ear infections. Viruses. Fevers. Sore throats. Parents can be forgiven for being overprotective, but according to pediatric emergency medicine doctor Christine Darr, some parents have a very good reason for coming to see her.
When seven-year-old Bayla Nelson came into the emergency department on a weekend a few years ago, her parents were concerned. The youngster had been feeling ill for eight days. She’d had a fever, been vomiting, and complained of a persistent headache. They’d taken her to see the pediatrician, but that doctor had given her IV fluids and thought she’d feel better in a few days. The following day, however, their daughter was feeling so poorly that her parents called the pediatrician back. The doctor advised them to visit the emergency room.
When Dr. Darr first laid eyes on the patient, she’d initially considered strep throat. Things like pneumonia and a urinary tract infection were on the physician’s list of possibilities as well. But a strep test, a urine dip, and a chest X-ray came back negative. One of the girl’s symptoms in particular bothered the doc. “Younger kids tend not to complain of headaches very often,” Darr says. “When a prepubescent child complains of a headache, it’s usually something to pay attention to.”
Darr did a quick test on Bayla’s eyes, specifically looking for her optic disc. It wasn’t visible—a conclusive sign of increased intracranial pressure. Darr wanted to order an MRI, but the test wasn’t immediately available in the ER on the weekends. She requested a CT scan of Bayla’s head instead.
The radiologist called with results 10 minutes later. A dark spot had turned up on Bayla’s left frontal lobe. Although the spot could have been a brain tumor, Darr felt the patient’s symptoms were more consistent with a brain abscess, a pocket of bacteria-laden pus, and started the girl on IV antibiotics. One of the most common reasons for an abscess is a severe case of sinusitis, but Bayla hadn’t experienced sinus problems. There had to be another reason for the abscess, even though the doctor knew finding exact causes for infections like these is rare. Darr called a pediatric neurosurgeon and admitted Bayla to the hospital.
After multiple procedures and tests, doctors determined Bayla had patent foramen ovale, a hole in her heart that had allowed bacteria to seep into her bloodstream. By happenstance, that bacteria set up residence in the girl’s brain.
“This stuff is what makes the job interesting,” Darr says. “The thing about emergency medicine is that there’s always something new coming in, so you have to keep your mind open to the possibility it could be something more than a cold or an earache.” Of course, these diagnoses aren’t common: In any given year, Darr says she makes only a handful of unusual diagnoses. But, as Darr points out, answers to medical questions are sometimes just the beginning. After Darr diagnosed the abscess, neurosurgeons inserted a drain to reduce the pressure in Bayla’s brain, and cardiac surgeons went in to sew up the hole in her heart.
Mystery Disease: Inflammatory Response
For more than 35 years, doctors at Children’s Hospital Colorado have been examining an illness that incites unpleasant symptoms in the youngest of patients.
About once a week at Children’s Hospital Colorado in Aurora, Dr. Mary “Mimi” Glodé sees a patient with the roster of telltale symptoms she’s come to know well: fever, irritability, swollen lymph nodes, rash, bloodshot eyes, a red tongue with small raised bumps, cracked lips, bright red palms of the hands and soles of the feet, stiff neck and joints, and peeling skin around the toenails and fingernails. It’s not a pleasant sight to behold. Especially since most of Dr. Glodé’s patients are younger than five years old.
About 50 children with these symptoms land at the Children’s Hospital each year. They are the fortunate few who end up at a health-care organization that has a long history dealing with their unusual illness. Dr. Glodé and Dr. James Todd are infectious disease doctors who’ve worked together for more than three decades. Glodé is an expert in treatment; Todd was the first American physician to describe the disease. “We published a paper back in 1976, almost simultaneously with three other papers from around the country, that this disease existed here in the United States,” Todd says. “The disease had been previously described by a Japanese pediatrician as mucocutaneous lymph node syndrome.” Today, it is more commonly known as Kawasaki Disease, an illness characterized by the inflammation of blood vessels in the body.
Although the mortality rate for the disease is generally listed as less than one percent, that statistic may be misleading. The most troubling—and lasting—effect of the disease (which affects about 5,000 Americans annually) is that about a quarter of those who contract it develop heart problems in the later stages of the typically three-week-long illness. “This is a disease that can cause coronary artery disease in young kids,” Glodé says, explaining that the prolonged inflammation can damage the heart’s vessels. “The initial symptoms of the disease burn out after a while, but we may actually be seeing adults having fatal heart attacks from having untreated Kawasaki Disease in childhood.”
Which is why Dr. Glodé is admittedly obsessed with not only treating everyone with the disease, but also seeking the cause of this mysterious syndrome. While experts agree there is likely a genetic predisposition—which would explain the higher frequency among those of Asian descent—they also posit the disease is triggered by an as-yet-to-be-identified agent, such as a virus or bacteria.
Kawasaki Disease often presents as a normal infection, something kids might pick up at preschool. They’ll have a fever. They’re irritable. They get a rash. Their lymph nodes are swollen. Even if parents are concerned enough to visit the pediatrician, the syndrome can be mistaken for scarlet fever, a staph infection, or even mononucleosis. And, to make it that much more difficult on your everyday pediatrician, there is no test for Kawasaki Disease. It is typically a diagnosis of exclusion, although doctors can check for mild anemia, a high white blood cell count, and an elevated erythrocyte sedimentation rate, which indicates blood vessel inflammation. All of which means many people may be suffering through the disease’s early symptoms as youngsters, only to experience dire consequences from the disease later in life as well. The only way to prevent this from happening? “If your child has a fever for more than five days and has two or more of the other symptoms,” Glodé advises, “get him to the doctor and mention Kawasaki Disease.”
Difficult Diagnosis: Cracking the Code
How a tiny piece of missing genetic material can have a huge impact.
Fair-skinned with a slight build, Dr. Matthew Taylor smiles a wry grin as he remembers Roger Evans’ first day at the clinic. “He came to us from an endocrinologist who wanted us to do some testing,” says the doctor, who is a genetics physician at the Adult Medical Genetics Clinic at the University of Colorado Hospital. “Roger was definitely a mystery.”
“I had a perfectly normal childhood,” Roger Evans says today. “I grew up in Southern California, went to school, and graduated on time.” Evans says he was rarely sick as a child, and except for some muscle spasms in his early teens—which his father chalked up to growing pains—he says he doesn’t remember being anything but healthy.
That began to change when Evans, now 51, matriculated into his later years of high school. “I guess I was old enough to notice that I didn’t look like my younger siblings,” he says. “My eyes were different; I had a round face; my ears were short. I actually asked my parents if I was adopted at one point.” Satisfied that he was a blood member of the family once his parents showed him his birth certificate, Evans forgot all about the differences he saw in himself and got on with planning his young life. He got a few odd jobs after graduating high school, but ultimately decided to enlist in the Army in his early 20s.
Although he was still experiencing some mild muscle cramps, he passed the Army’s physical exams. “It wasn’t until I got into basic training that I noticed I wasn’t really able to keep up with the other soldiers,” Evans says. “I was short-winded and fatigued.” He made it through eight weeks of basic before, during a 10-mile marching stint, he collapsed. Evans took a medical discharge from the Army weeks later.
During the years after the Army, Evans remembers feeling sick a few times and having general weakness, but he didn’t seek medical care. At least, not until he had his first seizure in 1984 at 24 years old. “The doctors diagnosed me with low blood calcium levels,” he says. Doctors prescribed calcium tablets. For the better part of a decade, Evans lived with low calcium–induced muscle spasms and weakness but nothing that stopped him from moving to Denver for a job with Continental Airlines. Then, in 1995, the seizures returned.
Tests for epilepsy came back negative. But, once again, doctors found his blood calcium levels were dangerously low. Calcium tablets just weren’t strong enough. They prescribed Rocaltrol, and surmised that his parathyroid glands, which control calcium levels, were not functioning properly. Evans remembers asking the doctors what might be causing the glands to malfunction—but no one seemed to know.
It wasn’t until three years later, at a Christmas Eve church service, that a particularly scary seizure prompted Evans to seek a solid diagnosis. “I had recently quit my job so I had decided to go back to school,” Evans says. “I realized that I needed to get a job and get medical insurance so that I could figure out what was wrong with me. I was almost 40 years old.”
But finding a doctor—and a diagnosis—was more difficult than he’d imagined. Evans went to an endocrinologist, who eventually told him his case was too complicated for her. He tried a primary care doc, who Evans says wasn’t able to control his blood calcium levels well enough to allow him to walk. Finally, years after he’d made the decision to find out what was ailing him, Evans opened the phone book and picked the first endocrinologist on the list. He had an appointment set for February 2003 with Dr. Margaret Eagan at Rose Medical Center.
“Dr. Eagan was the first doctor I’d had that tried to help me,” Evans says. “She took an interest in me. She started from scratch.” She diagnosed Evans with rickets, a softening of the bones typically due to a vitamin D or calcium deficiency. But Dr. Eagan then sent Evans to her mentor, Dr. Michael McDermott, at the University of Colorado Denver School of Medicine. McDermott disagreed with his former colleague, and diagnosed hypoparathyroidism leading to hypocalcemia, which essentially meant Evans’ parathyroid glands weren’t functioning. But Evans already knew that. He’d been on calcium pills—and then thrice weekly, three-gram IV infusions—for years. He wanted to know why his parathyroid glands weren’t functioning.
“I remember sitting back in Dr. Eagan’s office and asking her how we go about figuring things out,” he says. The doctor looked him over again; she examined his hands and ears and nose and eyes. Evans remembers Eagan, almost under her breath, saying that it could be something called DiGeorge syndrome, a disorder she’d only once heard about in medical school. Eagan then sent Evans to Dr. Matthew Taylor.
Taylor thought there were two possible genetic issues: one, a potential genetic mutation on Evans’ calcium-sensing receptor gene (CASR). The other, which Taylor believed was a more remote possibility, was for 22q11.2 deletion syndrome, more commonly called DiGeorge syndrome, which is a defect in which certain genes get deleted from an area along the larger arm of the 22nd chromosome.
“Roger didn’t have the classic presentation of 22q deletion syndrome,” the doctor explains. “Patients with that syndrome typically have cardiac defects, immune problems, feeding problems, and developmental problems.” Evans exhibited some of the typical facial features (low ears and wide-set eyes) associated with the disorder as well as the low blood calcium levels, but 22q11.2 deletion syndrome is almost always diagnosed early in life. Evans was 43 years old.
Taylor ordered a test for the CASR mutation, which six to eight weeks later came back negative. The doctor then sent off labs for 22q11.2 deletion syndrome. Nearly 30 years after Evans’ dad told him his muscle spasms were normal for a teenage boy, Dr. Taylor told him otherwise: Evans was positively diagnosed with 22q11.2 deletion syndrome.
“It was a long, hard road, but I was thrilled to have a diagnosis,” Evans says. “I had to be my own advocate sometimes, but I had so many little angels helping me. And I did learn that just because you get an incorrect diagnosis at first doesn’t mean you should give up—sometimes you just have to work through things with your doctor.”
Although he has his diagnosis, Evans does not have a cure. Since the positive lab results, he has learned he has other characteristics associated with the syndrome: specifically, three different heart defects. And because of his need for so much calcium, his kidneys have begun to fail. But he remains optimistic—and thankful. “I’m grateful for the good doctors, like Dr. Taylor, that I ultimately found,” he says. “So many people never know what’s wrong with them. At least I know.”
Medical Advice: Advocate for Yourself
How one woman learned never to settle when it comes to your health.
There’s nothing simple—or typical—about what Dr. John Mitchell does at the University of Colorado Hospital. Surgically removing damaged sections of lung through a small incision takes serious skill, yet Mitchell makes it sound so easy. “I’m familiar with techniques to deal with infection in the lung,” he says, “and I’ve been doing it a long time.” That may well be true, but what he does in conjunction with the folks at National Jewish Health is miraculous to his patients—especially Deborah Schwartz.
Schwartz, 62, lives outside Philadelphia, but she found medical salvation in Denver in 2010. Diagnosed with mycobacterial infection (similar to, but not the same as, tuberculosis) in 2004, she was put on antibiotics by her East Coast physicians. She lived well for two years before she began experiencing adverse reactions to her medications. Her doctors took her off the antibiotics. That’s when she started coughing up blood. “I needed more advanced care,” Schwartz says. “My doctors told me I was a perfect candidate for some doctors they knew about in Denver.”
Schwartz made the cross-country trip to see physicians at National Jewish. They recommended surgery with Dr. Mitchell, but when Schwartz decided she didn’t want to have surgery so far from home, she went back to Pennsylvania to see specialists. But no matter whom she spoke with, not one doctor was willing to offer what National Jewish and the University of Colorado Hospital were offering. “At first, doctors back East told me that they didn’t want to do surgery at all,” she says. “Then they told me that they couldn’t do the surgery thoracoscopically; they would be using a gigantic incision. And they also told me that no one could do the surgery safely the way the doctors in Denver wanted to do it.”
Schwartz’s story isn’t uncommon. Dr. Mitchell says he hears similar anecdotes often. “A lot of my patients express frustration with treatment they’re getting at home,” he says. “Debbie was experiencing suboptimal treatment options, and instead of giving in she fought for herself. She was determined to be proactive.” It’s a refrain that Mitchell—and now Schwartz—uses often. Although they’re coming from different perspectives, both stress patients’ need to learn to be their own best advocate when it comes to their health.
“I think people often go to one doctor and then that’s the doctor they go with,” Schwartz says. “People need to study, sit down at the computer and see what other doctors are doing.” Schwartz acknowledges she is fortunate to have insurance and the financial wherewithal to travel across the country to seek different treatments. However, she still advises others to know their options. “If I had gone with docs in Pennsylvania, I may not have been able to get surgery or I would’ve had a huge incision and a tougher recovery.”
Instead, Schwartz signed on with Mitchell for two minimally invasive procedures. A few days after each surgery Schwartz was shopping in downtown Denver, and today she is breathing much easier.