The Local newsletter is your free, daily guide to life in Colorado. For locals, by locals.
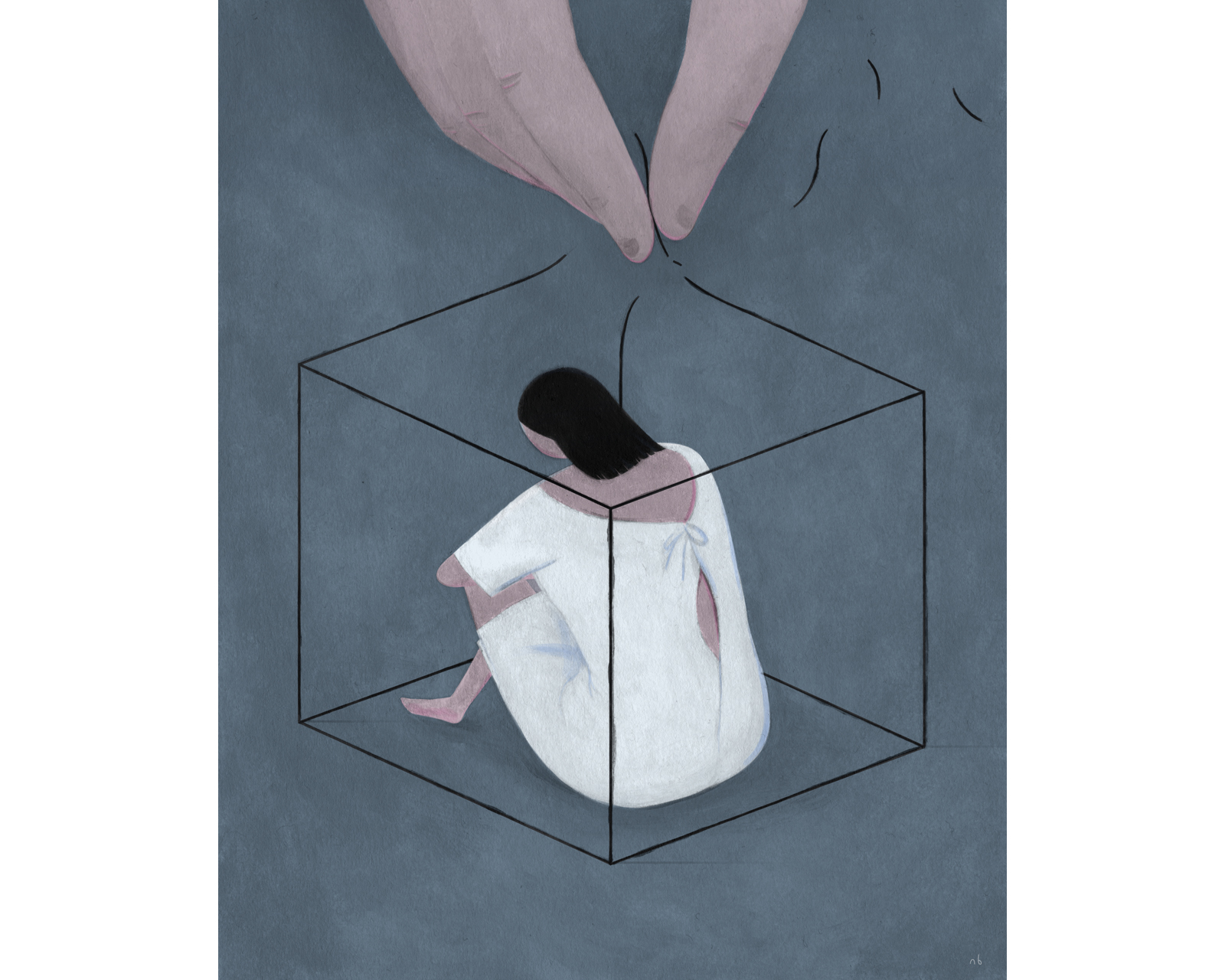
5-3-6. The numbers flashed repeatedly in Esperanza’s* mind to the tempo of the blinking red brake lights shining before her on the highway. What she wanted to be thinking about was her birthday; she had turned 23 the day before, and her friends were planning a party south of town. But all she could focus on were those three numbers. Less than an hour earlier, the man who employed her as a nanny in the Cherry Creek area had forced her onto his bed and raped her, she had told the friend now driving her to a hospital in the south suburbs. Esperanza says she remembers glimpsing the bedside clock—it read 5:36 p.m.—as she prayed for him to stop. Now, as rush-hour traffic on I-25 slowed to a crawl, she was sitting in her sundress in the passenger seat of her friend’s car holding her underwear in her hand.
When they finally arrived, Esperanza approached the front desk. She knew what had happened; she knew she represented a statistic, one of the 20 percent of American women who are victims of rape or attempted rape in their lifetimes. But it was hard to say the words out loud. She whispered so quietly that the intake nurse asked her to repeat herself. Then she sat down to wait. Soon, someone ushered Esperanza into an exam room, where the staff informed her that while they could address her injuries or other medical needs, they didn’t have any rape kits or nurses who could perform a specialized forensic exam. For that, Esperanza would need to go to the Medical Center of Aurora—16 miles away. (She turned down the hospital’s offer to transport her in an ambulance, knowing her insurance wouldn’t cover it.) She felt completely zapped of energy, she recalls, but her friend helped her back into the car, and they headed toward the highway once again.
Most sexual assaults—some estimates say as many as two-thirds—go unreported to police. The reasons for this vary from fear that the perpetrator will retaliate to the victim blaming him- or herself to misunderstandings surrounding reporting laws, which in Colorado recently changed to allow survivors to remain anonymous or seek medical help without involving law enforcement.
Esperanza wanted to tell the police. She knew her attacker and wanted him to answer for it. She’d already overcome one of the many barriers rape survivors encounter: She told someone what had happened, and that person believed her. But then she ran into an obstacle she never imagined. The hospital, a place whose mission is to help and heal, wasn’t equipped to assist her.
Hospitals are required by law to treat whomever walks through their doors, including victims of sexual assault. And while almost any medical professional can treat injuries or follow the steps on a rape kit, most of them haven’t been trained in the specific techniques required for a sexual assault medical assessment, which may include examining the pelvis, photographing injuries, and swabbing the vagina, anus, or mouth for DNA and other evidence. (If evidence is improperly collected, packaged, or stored, that mismanagement can have serious repercussions, like failing to meet the strict legal requirements that would help prove a case against an assailant.) The average medical provider also may not be proficient in trauma-informed care, which is why it’s preferable to send patients to a venue with staff who are specially trained.
This specialty for registered nurses emerged in the 1970s. Sexual assault nurse examiners (SANEs) undergo focused training in sexual assault trauma response and evidence collection; advanced medical professionals who are not registered nurses, such as physicians or physician assistants, can become sexual assault forensic examiners, or SAFEs. SANEs and SAFEs can be called as expert witnesses in court, and studies show that exams performed by these professionals often result in improved care for victims, higher-quality evidence collection, and better prosecution rates of perpetrators. Even still, a March 2016 report from the national Government Accountability Office found that there aren’t enough SANEs to “meet victims’ needs for exams.” And there are no federal requirements to train or employ SANEs or SAFEs in health-care facilities.
In Colorado, almost every judicial district has at least one of these specialized providers, though they’re concentrated in the seven-county metro area. Nine SANEs work in south Denver at two hospitals (Porter Adventist and Littleton Adventist), while Denver Health has 18. But because much of our state is rural, it’s not uncommon for a single medical forensic examiner to handle cases from multiple counties. Telluride, for instance, is more than an hour’s drive from the nearest specialist, in Montrose.
Hospitals and medical centers in many of these rural areas don’t see enough sexual assault patients to justify paying to staff an in-house setup. This is why all but one of Colorado’s programs are on-call operations, with many of the examiners working as SANEs in addition to their regular shifts as emergency department nurses. The extra hours—and intense nature of the job—can cause burnout, leading to fewer nurses when what survivors need is more. “Sexual assault doesn’t happen neatly between the hours of 8 a.m. and 5 p.m.,” says Lisa Ingarfield, sexual assault response program director in the Colorado Office for Victims Programs. “There’s a false connection that gets made: Folks don’t show up for the exams, therefore people assume sexual assault is not happening. It’s still happening.”
Colorado’s Division of Criminal Justice started the Sexual Assault Response Project in 2012 to address this shortage. In 10 rural communities, it created multidisciplinary sexual assault response teams (SARTs) whose goal is to streamline processes, establish protocols, and identify and fill any gaps in services, like possibly starting a SANE program. (The federal grant that funds this effort runs out in September; the Colorado Coalition Against Sexual Assault, a Denver-based advocacy and support group for survivors, has submitted an application in the hopes of taking over the project.) Still, advocates say we need to do more. And they point to one local hospital as the gold standard.
The sexual assault exam room at Memorial Hospital Central in Colorado Springs looks like any other hospital room, with its eggshell-colored walls and stack of pamphlets—until you look a little closer. Inside a white floor-to-ceiling cupboard sits a stash of rape kits. Next to the blue exam table is a large mobile microscope with a camera to do up-close examinations of a patient’s cervix. In a cabinet in the bathroom, comfortable outfits are folded into drawers, ready for survivors to wear after their clothing is taken as evidence.
This is where Memorial’s team of 12 SANEs saw 1,766 patients in 2015. And it’s the only hospital in the state—one of just a handful in the entire country—that runs an in-house, around-the-clock forensic nurse examiner program. “Every year our number of assault victims keeps going up,” says Megan Lechner, manager of Memorial’s forensic nurse examiner team. “Our rates have to do with us being here 24/7 and providers [such as law enforcement and other health-care officials] in our community knowing we’re here.”
Memorial’s SANE initiative was the first in Colorado. It started in 1995 as an on-call program before it began employing nurses full time in 2011. “The exam is very therapeutic,” Lechner says. “There’s someone recognizing [the person’s] trauma and reinforcing that it’s not their fault.” The hospital has also partnered with TESSA, a local nonprofit that provides confidential victim advocacy to survivors of domestic violence and sexual assault, so there is also an advocate available at all hours.
The SANEs at Memorial have recently extended their hospital-funded practice to include any victims of violence, including strangulation and human trafficking. The team also has a grant from the Division of Criminal Justice to provide statewide education; they run training sessions with law enforcement, public defenders, health-care providers, and others to educate the community about the program’s importance. “We’re not angels of mercy who swoop in and save the day,” says Kim Lee-Nash, the statewide SANE/SAFE trainer. “But we give [survivors] a little control back.”
Esperanza did eventually make it to the Medical Center of Aurora that July day in 2010. She was examined by a SANE, whom she recalls as kind and gentle. As Esperanza quietly cried, the nurse swabbed her mouth, took photos of bruises on her arms and inside her vagina, plucked some strands of her hair, and checked her pubic hair for evidence. At every step, the nurse asked for Esperanza’s permission.
Today, as she tells her story, Esperanza still displays some of the embarrassment and discomfort she felt that night. But she also recognizes that even with what happened and how her ordeal ended—her case went to criminal trial, where her alleged attacker was acquitted—she’s one of the luckier ones. She had the support of her mom and dad on the phone right after the assault and her friend driving her across town, and she was treated by a nurse who was compassionate and understanding. “They know they can’t fix you,” Esperanza says of the SANEs. “But they’re the first people [after the assault] to give you some self-worth. I felt I had control over my own body. I felt like I was really believed; there was no judgment.”
In May, U.S. Senator Patty Murray, a Democrat from Washington state, introduced the Survivors’ Access to Supportive Care Act, which would, in part, establish a national training program and increase access to SANE/SAFE services. The bill has been referred to committee but is otherwise stalled. Colorado’s efforts are similarly sluggish, though some progress has been made. “The state has been doing a really good job in addressing some key issues,” Ingarfield says, pointing, in part, to our new reporting laws and the increasing number of SANE and SART programs that have launched around the state. But it’s still difficult to get these programs going, she says: “You need a critical mass, or you need a hospital administration that is fully supportive.”
Esperanza believes these efforts are crucial for survivors’ physical and mental health. She knows how it feels to be shuffled between different medical workers and hospitals. “You feel like you’re not being heard,” she says. “No one should have to go to a second hospital. There needs to be a SANE program in every single hospital.”
*Not her real name.
YOU HAVE OPTIONS
Colorado’s reporting laws got an update in 2015: Adult survivors can now decide, with a few exceptions, whether to engage law enforcement and whether to undergo a medical forensic exam (at no cost to the survivor). Here, we outline the three options available.
1) Law Enforcement Report: The survivor reports the assault, undergoes a medical forensic exam, has the evidence tested, and is willing to consult with law enforcement.
2) Medical Report: The survivor opts to have a medical forensic exam performed but chooses not to engage with law enforcement at the time of the exam. The evidence and the survivor’s name and contact information are handed over to police, but the survivor decides whether the evidence gets tested at that time; if he or she decides not to have it tested, it will be stored for at least two years, during which time the survivor can request a test. At any time, the survivor can decide to file a police report.
3) Anonymous Report: This is the same as a medical report, except the evidence turned over to police is released with a unique tracking number instead of the survivor’s name and contact information. If the survivor has a change of heart, he or she can contact law enforcement with the tracking number to file a police report. At this point, the evidence will likely be tested.
GET HELP
Find resources through the Colorado Coalition Against Sexual Assault, ccasa.org, and TESSA, tessacs.org.